
Around 90 people with connections to the Greater Manchester and Eastern Cheshire Strategic Clinical Networks (GMEC SCNs), came together to mark its 10th anniversary.
Clinicians, policy makers and other staff, present and past, got together to look back at the achievements of the Greater Manchester and Eastern Cheshire Strategic Clinical Networks, as well as discuss the future of Networks.
Director Julie Cheetham (pictured above) and Dr Peter Elton (pictured below right), clinical director, opened the event by expressing pride in how the networks have widened clinical involvement with more than 60 clinical leads, advisors and associates, ably supported by a great team of project managers and other staff.
|

Julie said: “It was a very positive afternoon. We knew it was important to say ‘thank you’ to our hard-working, innovative and ambitious clinicians, as well as pause to reflect on what we have achieved over the past 10 years.”
Peter said: “The commitments of clinicians and staff is amazing. It was great that the afternoon was spent reminding ourselves how well we can do when we work together using the expertise of our clinicians.”
The event was supported by the Royal College of Physicians of Edinburgh.
Click to read the event programme.
|
Each of the networks presented highlights of their work showing how they had changed the lives of patients for the better.
Both clinicians and support team members took to the stage to tell their stories, with passion and keen focus on the need to improve services for people.

Julia Birchall-Searle and Dr Carol Ewing from our Children and Young People Network talk through the team's journey since 2013, highlighting the work during the pandemic and the asthma friendly school programme.
|

Eileen Stringer, clinical lead midwife, and Each Baby Counts lead midwife Chloe Hughes, explain the work and successes of the Maternity Network, which has been a part of the GMEC SCNs since 2013.
Each Baby Counts aims to improve psychological safety, culture and escalation behaviours to reduce stillbirths and brain injuries caused by labour.
|
 |
|
Our clinical lead for the Cardiac Network, Professor Farzin Fath-Ordoubadi, spoke to guests about the amazing improvements to access to angiography, meaning every person in the city region has the same route into some of the best care in the country.
|
Dr Sanjay Sastry, also from our Cardiac Network, spoke about the importance of many different stakeholder groups coming together with clinicians to formulate policy.
|


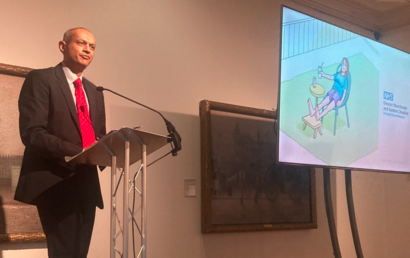
Next was the Diabetes Network, which entertained the audience with a Play Your Cards Right-inspired game, based on diabetes statistics in Greater Manchester. Dr Naseer Ahmad is pictured on stage.
|

The Diabetes Network clinical lead Dr Naresh Kanumilli spoke about the team's achievements over the past decade.
|

Dr Raja Murugesan, the Respiratory Network's clinical lead, spoke about one of the newer Network's history so far, giving a special mention to the long Covid projects.
Raja said it became clear they "had to do something" to help people with symptoms.
|

Sarah Rickard, manager of the Greater Manchester Neurorehabilitation and Integrated Stroke Delivery Network, told guests that patients in the city region enjoy services 10 years in front of some other areas of the country.
|

"Greater Manchester is in a much better place than many other parts of the country," said Professor Martin Vernon, clinical lead for our Frailty Network, talking about services for patients in our city region.
|

The Palliative and End of Life Care Network's quality improvement manager Elaine Parkin dedicated the session to Tony Bonser, a carer representative who helped bring the carers' voice into this area of healthcare and supported the work of her team. He sadly died in December 2022.
|
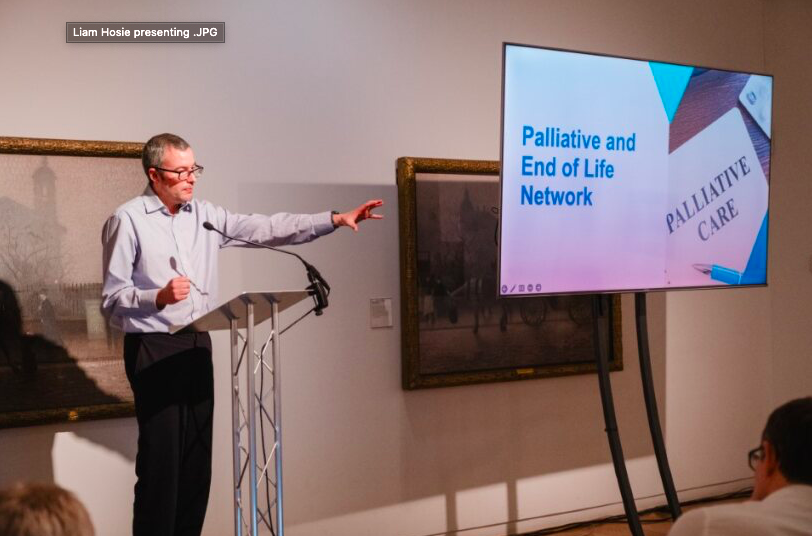
Dr Liam Hosie, Wigan GP and the Palliative and End of Life Care Network's clinical lead, led an exercise in the room about advance care planning and focused on EARLY - a tool to help primary care identify people in the last year of their lives.
|
 A key part of the day was guest motivational speaker, Steve Head, who emphasised it was as important to celebrate achievements as reviewing when things go wrong.
He said we need to move forward by acknowledging the progress we have made, so that we can take even greater strides forward.
With so many clinicians and support teams carrying out the work of the GMEC SCNs, it very rarely unites, so the event was a good opportunity to catch-up, as well as engage with stakeholders.

Pictured above: NHS Greater Manchester Integrated Care chief executive Mark Fisher and the GMEC SCNs' clinical director Dr Peter Elton.
 Pictured above: Dr Akila Anbazhagan and Val Clare.
 Pictured above: Members of the Diabetes Network, left to right, Dr Sarah Steven, Dr Naseer Ahmad, Krista Williams, Dr James Hider, and Adam Wallis.
Pictured below: A selection of photos from the event, including the birthday cake, created by Fran Carbery, our Children and Young People Network programme manager.

 |



Dr Bill Kirkup CBE, who recently led an independent investigation into East Kent Maternity Services, visited Greater Manchester this month to speak to the Local Maternity and Neonatal System.
Talking to a range of colleagues from maternity and neonatal services, both clinical and non-clinical, and service user leads, Dr Kirkup held several sessions, focusing on improving services.
Colleagues are working incredibly hard to deliver the best possible services to our women, birthing people, and families. It was an opportunity for some of them to learn from his expertise and to reflect on things we could do differently.
Lively discussions took place about how we could focus better on tracking outcomes and developing escalation of early warning systems. There was also lots of focus on how we can improve culture and behaviours within services, supporting our colleagues with training and professional development opportunities.
Improving safety and outcomes is a key priority for our LMNS.
If you are interested in the work of the LMNS, please visit our dedicated LMNS web pages where you can find a dedicated section on safety, amongst many other things.
Dr Kirkup was also chairman of the Morecambe Bay Investigation in July 2013 and has also led investigations into the Oxford paediatric cardiac surgery unit.
Pictured above: Alison McGovern, associate director of the LMNS, Julie Cheetham, director of the Greater Manchester and Eastern Cheshire Strategic Clinical Networks; Dr Bill Kirkup CBE, Valerie Clare, clinical maternity assurance lead.
|

The North West Maternal Medicine Network has just released the first issue of its newsletter.
The bulletin is aimed at both clinicians, birthing people and their families and gives people information about what it does, where it operates, its key objectives, patient stories and dates for your diary.
Read the newsletter.


Dr Carol Ewing, pictured left, has just retired, after being a clinical adviser for the Children and Young People Network since our launch in 2013, when we were part of the Greater Manchester, Lancashire and South Cumbria Strategic Clinical Networks.
In this Q&A, she looks back at her work with us; a journey which has included the opportunities of devolution and the challenges of Covid.
|
What is your career background?
I trained at the University of St Andrew's and then at the University of Manchester and I qualified in 1978. My first training post was at North Manchester General Hospital. My postgraduate training took place mainly in Manchester but also in Scotland and Liverpool.
I’ve been a Consultant Paediatrician with a special interest in atopic eczema and allergy since 1993. I worked in Manchester, firstly at Booth Hall Children’s Hospital in an innovative job-sharing partnership with Dr Eileen Baildam, Consultant Paediatric Rheumatologist until 2005. I continued to work at Booth Hall, moved to the new Royal Manchester Children’s Hospital in 2009 and I retired from clinical practice in 2019.
From 2019, I chaired the Greater Manchester Children’s Health and Wellbeing Stakeholder Forum which has brought together children and young people, parents, carers, volunteers, providers and commissioners and health and care professionals with a passion for working together to improve health outcomes and reduce health inequalities for our children and young people (CYP).
From 2020, I also co–chaired with Chris McLaughlin, OBE, Stockport Council’s Director of Children’s Services, the Greater Manchester Children’s Health and Wellbeing Executive Board, which oversaw the implementation of the GM Child Health and Wellbeing Framework, in particular, the physical health transformation programmes, which helped to maintain connections with other health and sector wide programmes for CYP, during Covid.
In previous professional honorary roles, I was the Royal College of Paediatrics and Child Health (RCPCH) Workforce Officer 2009–2014 and RCPCH Vice President for Health Policy 2014-2019. I gained a lot of experience in these roles and this has helped me a lot in my GMEC SCNs clinical advisory role. Key highlights were to support the RCPCH in publishing a range of CYP service standards, to contribute to the early development of the NHS England (NHSE) CYP Transformation Programme and to co–lead with NHSE and the Royal College of Nursing, the initial development of a Paediatric Early Warning System which has been recently launched. In recognition of my services, I received an Honorary Fellowship from the RCPCH in 2021.
From 2019 until I retired, I have been the RCPCH Ambassador for Greater Manchester, combining this role with the Greater Manchester lead roles to advocate for child health and services and improve care and services given to children and young people.
(Carol, pictured right, speaking at the recent 10th anniversary event). |
|
 |
How did you become involved with the SCNs?
I joined the Networks in 2013 when they were established – I was appointed first of all as the clinical lead for the CYP Network and continued as a clinical adviser when I took up the post of RCPCH Vice-President for Health Policy.
As a clinician, I’ve always been passionate and privileged to try to help and support CYP and their families.
I have also had a great interest in improving CYP policy and advocacy, the CYP health service and its workforce, and that’s why I found the work of the Networks very inspiring and innovative. It’s forward thinking and tries to set the right standards and improvement programmes to provide the best care for children.
I strongly believe that the clinician’s voice and the children and young people’s voice, together, should be at the heart of decision-making - trying to make sure the influence comes from the people who are delivering care and those to whom we are providing the service.
How did things change with Devolution in Greater Manchester?
Before Devolution, the Greater Manchester, Lancashire and South Cumbria Strategic Clinical Network was established as part of the Health and Social Care Act - in 2015, funding was withdrawn.
What our Greater Manchester Clinical Network leaders did, which was again very innovative and forward-thinking, was to continue to support child health. Even though there was no funding, they kept our posts going. Then Devolution came along, and this was an opportunity to really embed our collective improvement strategies for child health in the Greater Manchester Health and Social Care Partnership (GMHSCP) work programmes.
So, the GMEC CYP SCN took its chance to address children and young people’s needs and improve their care through the GMHSCP. Jon Rouse, the chief executive at the time, was very passionate about improving services and improving outcomes for CYP and this really helped us to work with GM partners in our pursuit of developing better health care and services for them.
The Greater Manchester Child Health and Wellbeing Framework, to which I contributed, was approved by the GMHSCP Health and Care Board in 2018 – this set out how GM, as an integrated system, would aim to improve child health and wellbeing from 2018 to 2022.
One of the pieces of work I have also been involved in over the past few years has been to contribute to the development of a refreshed Greater Manchester Combined Authority (GMCA) led integrated Children and Young People’s Plan 2019 – 2022 – this has been closely aligned to the GM Child Health and Wellbeing Framework. The refreshed plan also links to the developing strategic, integrated and operational plans to improve outcomes for children and young people within the recently established GM Integrated Care System. In February this year, a Children and Young People Principles paper to which I contributed, was endorsed at the GM Integrated Care Partnership Board – this was a pivotal moment.
I have been working with the NHS GM Integrated Care children’s leads over the last few months to help with a smooth handover of any GMEC SCN or GM system wide programmes of work in which I have been involved, to inform the developing NHS GM Joint Forward plan.
My work as GM RCPCH Ambassador, and to embed CYP voice within all policies and programmes in GM, have been key parts of my handover to NHS GM.
What impact did Covid have on children and young people services?
Covid changed the direction of travel for the GMEC SCN. I was part of the team which contributed to all the work we did around Covid, which included making sure CYP’s health needs were part of the decisions being made, for example, workforce and service implications in response to the pandemic, winter planning and the GM all age recovery plan.
Unfortunately, we did see an impact due to Covid and the pandemic more widely on CYP’s health and wellbeing, including asthma admissions to hospital increasing after they had reduced in recent years; obesity levels have gone up too and mental health has deteriorated.
Covid was the biggest challenge I have seen in my professional life and it has had, and continues to have, an enormous effect on children and young people - we are trying hard to address its impact. However, CYP are very resilient too - we must not forget this and we must listen to what they say could improve their health and wellbeing.
Everyone across the health, care, education, criminal justice and voluntary sectors in GM are therefore trying to work collectively to help CYP recover from Covid, reduce its impact on their physical and mental health, enhance their health and development, their education and their other social opportunities so that we give them the best life chances they can have.
Do you think children and young people have been able to play a role in shaping programmes?
I am very proud of the role CYP have played and continue to play in developing our programmes, but of course we must go a lot further.
My starter for 10 is that any discussion about CYP should acknowledge that they have a right to be involved and we should always take note of their views. They can give you their lived experiences, shape health care and tell you whether the care you give works for them.
The GMCA-led Children’s and Young People’s Plan has a designated CYP voice and views section which I co–lead with Jacob Botham CYP Lead, GM Public Service Reform Team, GMCA and Stu Dunne, CEO of Youth Focus Northwest. We are taking a strategic approach to embed CYP voice and views in everything we do which affects them. We are making sure that people who work with CYP are trained to be able to listen to them. We are using a child rights-based approach to training called the Lundy model which is based on the UNCRC Article 12.
Every child has the right to express their views, feelings and wishes in all matters affecting them, and to have their views considered and taken seriously.
What would you consider having been the best achievement of your time at the SCNs?
I am probably most proud of the GM Child Health and Wellbeing Framework. It stretched further than health and linked up with established early years and mental health programmes, as well as further enabling partnership working with the Education and other Sector colleagues.
The Framework was highlighted as an example of good practice at national level in the early days of the development of NHSE’s integrated care systems.
I’m particularly proud of the work we took forward on the CYP’s voice as part of the Framework. The CYP produced a Charter, which they decided to call a Youth Agreement, underwent training and now go off and inspect child health services and feed back to each individual service, as well as the GM system. This is called Bee Counted. Here is their latest report.
The Framework, which came to an end in 2022, has been a strong step and link to the GM Children and Young People’s Plan and the developing NHS GM Joint Forward Plan (JFP) which will be for CYP up to the age of 25 years.
JFP’s priorities from a health perspective, and by working through a lens of inequality and the CYP voice, are to reduce asthma admissions, improve healthy weight, speech, language and communication, and join-up the physical health care we give with mental health and population health programmes.
As plans develop and are implemented, it will be crucial to capture the views and experiences of our CYP – I really hope that we see an improvement in their health and happiness and in their experiences when undergoing health care, particularly after the detrimental impact of Covid and the pandemic.
As an absolute ‘must do’, we all need to work together to improve the care and services we provide and to tackle inequality by addressing the social determinants of life to improve the health and lives of our children and young people.
What do you hope the future holds for the Networks?
One of the biggest challenges ahead will be for the GMEC SCN CYP team to continue to make the case, alongside mental and population health and sector partners, to move resources to equitably fund services which provide health and care for children and young people.
The shift of resources needs to be to areas of preventative care and through early intervention measures so that children start life in a healthy and happy way and continue to be healthy and happy.
This is a fundamental principle within the refreshed GMCA led CYP plan and which must be at the heart of the evolving NHS GM Joint Forward Plan.
As a key part of this, the GMEC SCN can play its part through its programmes to set out strategic recommendations on how to improve health by tackling inequality and by continuing to co-produce its programmes with CYP and families. These need to be across the GM system, localities and neighbourhoods, by supporting our CYP right through their lives from birth to young adulthood and by making sure they have the best opportunities they can receive.
The SCNs can continue to build on their strong foundations to bring the clinical voice across all organisational and sector boundaries, to support the GM CYP programmes being clinically led.
The GMEC SCN CYP team will continue to work with other sector partners to improve where CYP grow up and the environment around them, their education, and advantages from social activities. It’s not just about health but embedding their health improvements within a much wider system.
What are you planning to do during your retirement?
I will be 70 in December this year. This is my 45th year in the NHS and it is time to move on to new adventures, particularly to spend more time with my husband and family including our wonderful 4 grandchildren.
I have been very privileged to work as a member of the fantastic GMEC SCN team and of course in the NHS for many years - long may the NHS continue.
I intend to keep on advocating and lobbying on a voluntary basis for the rights of children and young people in GM by working with my GM CYP voice lead colleagues. I feel it is my moral and ethical duty to do so as many CYP and their families in GM experience hardship through the cost-of-living crisis, increasing fuel bills, the impact of climate change and as winter approaches – all which affect the health of our CYP.
I want to keep up good levels of fitness and will continue my annual target of taking part in the Greater Manchester 10k run for as long as I can and raise money for charity. My husband and I ran this year for Médecins sans Frontières.
Lastly, music has always been part of my life. I played the oboe as a young person and recently took up playing Irish music on the tin whistle! I really look forward to playing in a session but there is a fair bit of practice required to get there!
Dr Ewing asked us to signpost people to a story book, which was used during her presentation at the 10th anniversary event and tells the story of the CYP Network.
Read it here.

|