
Goodbye to a good friend
Elaine Parkin, quality improvement programme manager, Palliative and End of Life Care Network, pays tribute to Tony Bonser, a carer representative who she worked with for many years.
(Pictured above: Elaine is pictured above centre, to the right of Tony and his wife Dorothy).
“It is with a heavy heart I write this, but with a heart full of admiration for Tony Bonser, who sadly died on December 9, 2022.
Tony has been a long-standing carer representative to the Greater Manchester Palliative and End of Life Care programme following the death of his son Neil.
I have worked with Tony over the last 10 years and been witness to the enthusiasm and drive to improve and enhance palliative and end of life care services regionally and nationally.
Tony has been a great inspiration, speaking at many of the Strategic Clinical Network events and representing the North West as the lead for the National Dying Matters campaign. Tony would never turn down an opportunity if it made just one person stop and consider end of life care services or have a conversation and share it regarding their own personal wishes for end of life care.
Tony was passionate about encouraging and opening up the conversation about death and did this with such compassion and honesty.
I always looked forward to hearing Tony speak and address an audience as he had a way of motivating his audience and I always came away with a new idea or piece of work that would really make a difference to people approaching or at the end of life and those close to them.
Tony has influenced many improvements nationally for palliative and end of life care including his contribution to the development of the National Ambitions for palliative and end of life care; a recommendation for integrated care boards to meet their statutory responsibility to commission palliative and end of life care services for their population.
Whilst I will miss Tony in a professional capacity, I will miss his friendship, kindness, laughter, and pure enthusiasm for life and for making the life for those around him better.
Tony’s legacy will be long-standing in Greater Manchester, the north west and nationally, by the foundations he has laid in bringing the carers voice into palliative and end of life care.
For one last time, ‘thank you’ Tony.”

 The Network was back at the British Muslim Heritage Centre this month for an event called ‘Palliative and end of life care summit | a right or a privilege?’.
The event brought together more than 120 colleagues from across Greater Manchester and patient representatives to talk about palliative and end of life care. This was the Networks’ first large in-person session since before the pandemic.
Chaired by the Network’s clinical lead, Dr David Waterman (pictured below), the day was a chance for colleagues to hear from a line-up of fantastic speakers. The full list of which you can see here.

A few notable moments:
- Professor Bee Wee, national clinical director for palliative and end of life care, reflecting on the strengths of our approach in being grounded in strong clinical leadership, collaboration and a focus on quality improvement.
- The Greater Manchester Hospices Collaborative speaking about their invaluable contribution to the health and care system. Combined, Greater Manchester hospices have more than 1,000 staff looking after around 10,000 people every year, supporting people to live until they die. It prompted discussion about the way hospices are funded with concerns expressed about the forecasted deficit and impact this would have.
- Two powerful stories from patients about their experiences of palliative and end of life care.
- Andy Burnham, Mayor of Greater Manchester, arrived at the end of the day. Andy spoke about his vision for public services and his hope in the future for mental, physical and social services to be equal, lending his support to the importance of our work in improving palliative and end of life care for the people of Greater Manchester.
You can read through our Tweets from the day via #GMECEndOfLifeCare.
|

 A five-year action plan has been launched to improve maternity services for all communities.
Called the Greater Manchester Equity and Equality plan, it recognises some of our maternity services are not where they should be and sets out what changes need to take place.
For example, stillbirth rates increased during the pandemic and have not yet returned to pre-pandemic levels or align with national averages.
Also, some people in our region are experiencing disproportionately worse outcomes, based on their circumstances or protected characteristics, such as ethnicity, faith, belief, sexual orientation and disability.
A broad group of stakeholders, including people who use services, have been involved in developing an action plan that describes the things we will do over the next five years to improve maternity outcome measures and address health inequalities in Greater Manchester and eastern Cheshire.
More than 363 individual actions have been identified and some of the key priorities can be summarised under the following headings:
- Restoring NHS services following the pandemic inclusively
- Mitigate against digital exclusion
- Ensure data sets are complete and timely
- Accelerate preventative programmes that engage those at greatest risk of poor health outcomes
- Understanding the population and co-producing interventions
- Action on maternal & neonatal mortality, morbidity and experience
- Action on perinatal mortality and morbidity
- Provide support for maternity and neonatal staff
- Work with system partners and the VCSE sector to address the social determinants of health
- Strengthen leadership and accountability
Every person involved in maternity and neonatal services has a part to play to successfully deliver the changes needed.
Read the action plan, which runs from 2022-2027.
If you have any questions or want to get involved, please contact gmec.lmns@nhs.net.


Patients awaiting cardiac surgery in Greater Manchester will be given additional peace of mind thanks to a new home monitoring service.
Those being supported by the new service will be given equipment, including a device which they can use to input daily information such as their blood pressure.
They will have a direct link to a team of clinicians who will help them to manage their condition at home while at the same time allowing them to get on with their lives.
The service will be available to people waiting for specialist cardiac surgery, coronary artery bypass grafts or valve replacement, which takes place at Manchester University NHS Foundation Trust.
Launched last month, this new service has been developed by the Greater Manchester and Eastern Cheshire Clinical Network’s Cardiovascular Network, Manchester University NHS Foundation Trust and FCMS, a community healthcare provider. The equipment is being provided by Docobo, which specialises in remote monitoring technology.
Professor Farzin Fath-Ordoubadi, consultant cardiologist and the Network’s clinical lead, said: “For people with complex cardiac conditions, remote monitoring, supplementary to clinical care, can potentially improve health outcomes.
“Thanks to this technology we are able to have a direct link with the patients and be able to early detect any deterioration in their health condition.
“Patients showing deterioration will be identified, prioritised, and offered support as appropriate.
“As the waiting list for life saving cardiac surgery has grown, we have to identify those patients who are deteriorating and offer earlier intervention when needed.”
Natalie Marsden, from FCMS, said: “We see this as a ‘safety net’ service while patients are waiting for their surgery, and so that patients have that point of contact. Because of the pandemic, a lot of people on cardiac waiting lists may have been deteriorating for some time and have not necessarily gone to the GP.
“We are already providing this service in Blackpool and we find that people get to grips with the service really quickly and get comfortable with it. We recently flagged up a patient who had really bad chest pain and shooting pains, we advised him to call 999 and escalated to a consultant.
“He only went to hospital because we were in touch with him. This was really helpful for the family as they felt reassured that this was followed up and we are there as a service.”
Dr Manisha Kumar, Chief Medical Officer of NHS Greater Manchester Integrated Care said: “I’m pleased that this project is now starting in Greater Manchester.
“Across the NHS we are working hard to tackle waiting list backlogs and to make sure patients receive the care they need in the right place, as quickly as possible. It is great to see initiatives like this designed to support people while they wait for surgery.”
Going forward, patients will be given the option to opt into the service at their initial consultation with the cardiac team. Their consultant will explain the benefits of the service and, should they choose to take part, the FCMS team will contact the patient to arrange the next steps.
People living in Greater Manchester waiting for planned hospital care can also access general information and advice while they wait at www.whileyouwait.org.uk
|
A cardiac physiologist recruitment event is being held tomorrow (Wednesday, February 1) to help people discover opportunities at NHS Manchester University NHS Foundation Trust.
The event is at the Northwest Heart Centre, Wythenshawe Hospital, Manchester M23 9LT, from 9.30am-4pm.

The Network’s clinical leads and associates have led the creation of a new handy online guide to help parents keep their young children safe and well this winter.
The booklet is packed full of tips and information on how to keep little ones healthy, what to do if they become unwell, and the best place to go for expert advice and help. With many families facing the challenge of rising costs this winter, it also includes details on how to find a food back and where to go with money worries.
The nine-page guide, titled ‘3 Steps to Keep Healthy and Safe this Winter’, can be downloaded via this webpage. Please send the link to people who may find the information useful.
It offers tips on everything from putting a first aid kit together, to being aware of common illnesses, and the best room temperature for sleeping babies – plus the latest advice on Strep A.
The booklet also highlights that many parents or carers can get free food and vitamins for young children if they qualify for a Healthy Start Card – thousands of vitamins are waiting to be claimed in Greater Manchester!
It also has clear instructions to help parents and carers decide whether to take their child to their pharmacy, GP or hospital if they become unwell.

Would you like to earn £15 per referral and £15 for every person that starts the NHS Low Calorie Diet Programme?
Would you like to find out how Xyla’s engagement team can support your practice to identify, contact and recruit people into the programme?
Could you benefit from support and guidance with the medication changes that people need to make before starting it?
If the answer to any of the above questions is yes, then we would like you to join our Low Calorie Diet Programme webinar on Monday, February 27, at 4pm to hear about our programme for people with type 2 diabetes and the support available to practices in GM.
We would like you to join us on the webinar to:
- Gain a better understanding of the programme
- Learn how to identify and refer eligible people and the support available to practices form the Xyla engagement team.
- Hear strong clinical advice to increase confidence about completing the referral form
- Learn about the referral payment scheme and other incentives available to practices
Dr Manisha Kumar, chief medical officer NHS Greater Manchester Integrated Care, as well as local GP, will open the webinar which will also include a presentation from Dr Naresh Kanumilli, Greater Manchester diabetes clinical lead and GP, Anna Agar, contract liaison officer for Xyla, and Helen Bowker, diabetes specialist nurse, Heaton Moor Medical Group.
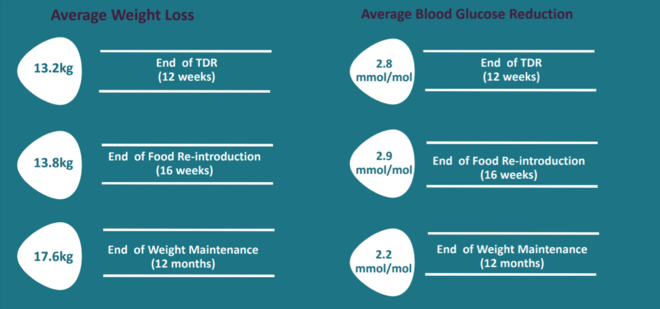
The FREE NHS Low Calorie Diet Programme is a new and innovative service for people with type 2 diabetes, helping people across Greater Manchester to lose weight, improve glycaemic parameters and potentially achieve remission of Type 2 Diabetes (see the table above for statistics on average weight loss and average blood glucose reduction).
We are seeing fantastic results for people across Greater Manchester and are offering up to £30 to practices for each person who starts the programme on top of incentives available to practices through the weight management DES.

The national stroke team is rolling out a programme called Stroke Quality Improvement in Rehabilitation (SQuIRe) across the 20 Integrated Stroke Delivery Networks in England.
It aims to support implementation of the integrated community model that was pioneered in our region and has now been successfully implemented across Greater Manchester.
The North West SQuIRe lead, Julie Emerson, has been working with the Network to support enhancing community rehabilitation and life after stroke support. The projects she is focusing on include:
-
Vocational rehabilitation (including return to work) – a North West network working group has been established to take a regional perspective for both stroke and neurorehabilitation and a training need has been identified and delivered. Data collection is underway to understand the need for vocational rehabilitation services. Next steps are agreeing a high-level pathway to support the models of delivery of more specialist support for vocational rehabilitation.
-
Advanced practice – the Network is working in Lancashire and South Cumbria and Greater Manchester to develop Advanced Clinical Practice (ACP) roles in stroke services. It has peer support sessions established by Greater Manchester that are open now to others in the North West to facilitate the development and retention of ACPs. It is currently collating case study exemplars of our advanced practitioners in both specialties. The Network will be working with our local and national universities to look at implementing the soon to be published Neuro rehabilitation and stroke capabilities framework (University of East Anglia)
-
Technology in rehabilitation – there is potential for a range of apps and technology to be used by clinicians to increase the frequency and intensity of rehabilitation for patients. A new project will look at barriers and facilitators for teams. The Network will develop a plan to address the barriers and produce a readiness for technology resource for teams to promote uptake
The national team also ran a funding call to help pump prime and pilot projects that would support implementation of the community model. The North West had around £1m of investment on offer and 14 “Catalyst projects” were funded with 6 going ahead in GM.
The successful applicants are currently completing projects plans and Julie has established a community of practice to support individuals and teams and to promote learning. The Greater Manchester Integrated Care Board has supported the Catalyst process and has agreed to review the outcomes of the projects. If you would like to discuss any of this work further, please contact Julie via julie.emerson5@nhs.net

|