November 2024

Acknowledge Lung Cancer Awareness Month this November by educating your patients on the risks and the importance of early detection and prevention. Smoking is the leading cause of preventable death in the U.S., and this month is a reminder that the healthiest choice to make is to quit.
Quitting smoking isn’t easy. You can help your patients through their quitting journey. Whether it’s their first or tenth attempt — continue to encourage them and provide them with the resources to quit. Lung Cancer Awareness Month is the perfect time to reinforce these efforts and remind your patients that smoking is the cause of about 90% of lung cancer cases. While quitting smoking isn’t easy, surviving lung cancer is harder.
The Oklahoma Tobacco Helpline can support your patients by offering nicotine replacement therapy such as patches, gum or lozenges. These can double their chances of successfully quitting. They get a free supply when they sign up with the Helpline.
Plus, be sure to inform your patients about the Great American Smokeout. Hosted by the American Cancer Society on Nov. 21, this event gives smokers the opportunity to make a plan to quit or use that date to begin their quit journey. Your patients can decide to quit solo or with friends, family or co-workers. Even if they choose to quit by themselves, they’re not alone. Every year thousands of people use this event to start living smoke-free!
Get the conversation started with free Helpline materials for your office. You can order your supplies at OKhelpline.com/order.

Please update your Oklahoma Health Care Authority (OHCA) provider files to ensure all details, including new or missing locations and group member assignments, are accurate. If your update impacts services under SoonerSelect partners, email your application tracking number (received upon submitting your update on the OHCA provider portal) to providerenrollment@okhca.org with "SoonerSelect update" and your application tracking number in the subject line.
OHCA has extended the expiration date of physicians from Oct. 31, 2024, to Nov. 30, 2024. This will allow provider enrollment time to process incoming renewals without interruption of services to members. There are currently more than 18,000 physicians who have yet to renew their Oklahoma Medicaid contract. To avoid any delay in reimbursement, physicians are encouraged to submit renewals as soon as possible. You can log into the provider portal to complete your renewal. If you need assistance logging into the provider portal, please contact our internet helpdesk at 800-522-0114, option 2, option 1. Or email SoonerCareInternetHelpdesk@gainwelltechnologies.com.
For the following provider types, 75-day renewals started Oct. 17, and contracts expire Dec. 31, 2024.
- Free-standing dialysis center
- Medicare crossover claims
- Treatment parent specialists (QBH I/II)
Please be sure the contact information, including email address, is current for all individual and facility/group provider files so you can quickly receive important contract information.

More than half of Oklahoma is a maternity care desert, according to the American Academy of Family Physicians and the March of Dimes. And only 8% of Oklahomans eat the recommended amount of fruits and vegetables. With those two co-occurring challenges, it’s easy to see the importance of emphasizing good nutrition and prenatal vitamins for pregnant and postpartum members.
SoonerCare covers dozens of prenatal vitamins at no cost to female members who are 10 to 50 years old, and the prenatal vitamins do not count toward monthly prescription limits. Many prenatal vitamins are available without prior authorization. SoonerCare also covers additional services for pregnant members in certain circumstances. For more information, visit the SoonerSelect health plan websites and utilize the resources within the provider portals. If you have questions about prenatal vitamins coverage or preferred prenatal vitamins, please call the pharmacy help desk associated with your patient’s health plan.
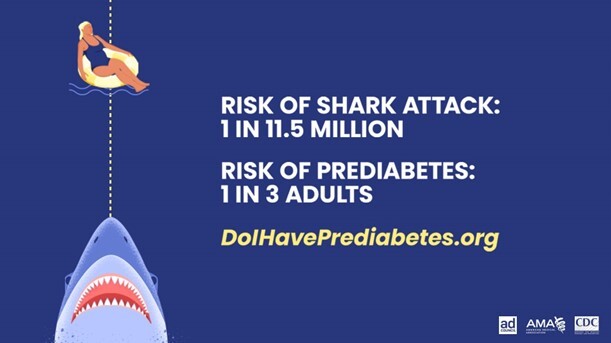
November is Diabetes Awareness Month, and it’s the perfect time to remind your patients to live a healthier lifestyle! With SoonerCare, your patients have access to Diabetes Self-Management Education and Support (DSMES) services, empowering them with the knowledge and skills to manage diabetes effectively.
DSMES Services
-
Learn and Apply: DSMES provides tools to monitor glucose levels, teaches healthier eating habits, and ways to stay active.
-
Prevent and Manage: Provides education on the risks and how lifestyle changes can prevent or manage diabetes.
-
Support Network: Connects your patients with health care professionals for continuous guidance and support.
SoonerCare is here to support your patient’s journey to developing and keeping healthy habits. Watch this webinar to learn more about DSMES.

2024 Global Messages
Oklahoma Health Care Authority has a page devoted to provider updates, global messages, provider letters and more. You can also subscribe to global messages so you will be alerted immediately of any important changes.
CE Contract Reminder
The SoonerSelect dental contract at Section 1.7: Covered Benefits and Section 1.8: Dental Services Utilization Management states that dental contracted entities (CEs) may not impose prior authorization guidelines/criteria or utilization management practices that are more restrictive than OHCA without OHCA prior approval. Have questions or concerns? Reach out using the contact information below.
Claim Status
For claim status and inquiries, please contact the OHCA call center at 800-522-0114.
Prior Authorization Inquires
Please contact the dental unit at 405-522-7401 if you have any questions or concerns regarding prior authorizations. The customary processing time for all prior authorization requests is six weeks.
Prior Authorization Amendments
If you wish to update orthodontic bandings or request any changes to a current approved prior authorization, you may do so by logging the provider portal, select “view original request,” then attach the form DEN-7. Please ensure this form is completed before uploading.
Checking Member Eligibility
Please ensure your office staff is checking member eligibility the day the member is in your office and prior to performing any services. A prior authorization does not guarantee payment and, if services are rendered for a member that does not have eligibility, those services must be written off. The member will not be responsible. It will also be important for your office to note whether the member has or does not have a dental benefit plan (the day of service).
Provider Resources
Visit the provider section of OHCA's website and you'll find many helpful links and tips. It includes information on provider contracting, training, claim tools, policy and the OHCA call tree. Plus, the SoonerSelect provider page offers webinars, FAQs, job aid claims and much more.

Q. What should I be doing under the “Service Provider Information” section of the prior authorization portal?
A. When submitting prior authorizations (PAs) in the provider portal, you must enter mandatory information by the section in order. This process for PA submission only applies to the therapies PA submissions for patients under 21 years old.
- Enter the provider ID in the “Requesting Provider Information” section.
- Enter the Member RID number in the “Member Information” section.
- Leave the “Service Provider Information” section blank. Entering information in this section, will create issues when filing claims leading to a denial of reimbursement.
Complete the “Attachments” section.
Q. What should I do if a member undergoes a name and associated RID number change?
A. When a member has an active PA for services and undergoes an RID number change, then an RID change amendment will need to be submitted using an HCA-60 amendment form. This amendment will create a new PA under the new name and RID number. OHCA will batch this new PA to you.
The form must include:
- The old RID number
- The new RID number
- The new start date (date the name change went into effect)
- The same end date as the original PA request.
- The number of units remaining that need to transition over to the new PA. For example, if the original PA had 60 units on line A and 45 units had been used to date, then you would enter 15 units on the HCA-60 form.
We recommend that all claims prior to the name change be completed before submitting the RID change amendment. This will ensure proper reimbursement for services before the name change, and consistent continuation of services after the name change.
Q. When is a Change of Provider form necessary in a PA submission?
A: A Change of Provider (COP) form will be necessary whenever services are transfered from one clinic to another (as services will no longer be under the same provider ID). The prior clinic is responsible for ensuring an appropriate handoff to the new clinic. The new clinic is responsible for a timely PA submission meeting all documentation requirements (including an up-to-date progress note when necessary to ascertain continued medical necessity).
As CPT codes themselves cannot be approved at two different locations simultaneously, it is important to note that a COP form may be necessary more than once. For example, if an SLP eval request PA for CPT 92523 is submitted with a COP form, and it is approved (due to meeting the 6-month COP timeline and associated documentation requirements), then the subsequent SLP treatment request PA for CPT 92507 must also include the COP form.
Q. Do I need to list modifiers in my therapies PA submission?
A: Regardless of the profession (PT, OT or SLP), a primary modifier must be present in any therapy PA submission. Each line in a PA request for a particular CPT code must include a modifier that indicates the profession of service to ensure sufficient claims processing and reimbursement.
-
SLP requests: All lines should include the GN modifier.
-
PT requests: All lines should include the GP modifier.
-
OT requests: All lines should include the GO modifier.
For example, if a PT PA request is submitted with line A for 97530, line B for 97110 and line C for 97140, then each of these line must include the GP modifier to ensure proper reimbursement for services.
The GT modifier indicates that services were rendered via telehealth. It should never be included in a PA submission; however, it should be listed as a secondary modifier when filing claims. For example, if bad weather led to an SLP treatment session being delivered online, then the claims submitted for this session with use of line A for 92507 should include the primary GN modifier and add a secondary GT modifier.

Lisa is a longtime supporter of Oklahoma ABLE Tech. When she needed durable medical equipment (DME) for mobility issues, she knew exactly where to look for assistance.
Lisa received a gently used four-wheeled upright walker from the Device Reutilization Program. The walker helped relieve Lisa’s pain, giving her back her independence and allowing her to be more active. She can now participate in more professional and personal activities, including taking pain-free walks around her neighborhood. The upright walker also helps Lisa stand up straighter, which helps her breathe easier.
Lisa is grateful for Oklahoma ABLE Tech. “Austin and Meg responded [to my request] immediately,” she said. “This upright walker is absolutely what I needed. Thank you!”
The Oklahoma ABLE Tech Device Reutilization Program provides free DME to Oklahomans in need, regardless of income. The program is 100% donation based and relies on help from community donations to provide DME devices like walkers, blood pressure monitors, shower chairs and more. To learn more about the Device Reutilization Program or to donate a device today, To learn more or to donate a device today, visit the Device Reutilization page.
|