|
View this as a webpage
December 2023
Pregnancy Risk Assessment Monitoring System (PRAMS) is a surveillance project conducted by Centers for Disease Control and Prevention’s Division of Reproductive Health in collaboration with the Minnesota Department of Health (MDH). The PRAMS survey asks new moms about maternal behaviors, attitudes, and experiences before, during, and shortly after their pregnancies. Participants are residents who recently gave birth within Minnesota to a live-born infant during the surveillance year. Birthing people are sampled between 2 and 6 months after giving birth.
PRAMS highlights
- Minnesota PRAMS (MN PRAMS) met the CDC response rate threshold for 2021
- 2023 data collection began in June 2023
- The new phase 9 survey and the web survey module also started in June 2023
This quarter’s newsletter focuses on postpartum depression (PPD) featuring topics such as the prevalence of PPD, disparities faced, obstacles to receiving care, and stressors experienced. Information on treatment and resources for support are provided, as well as recommendations for diminishing disparities and improving health outcomes for birthing people affected by PPD. Birthing people are noted as women for this report, but include all people who gave birth.
Postpartum depression and missed opportunities for earlier intervention
PPD is a common but serious mood disorder that affects pregnant people after their baby is born. Individuals may experience profound feelings of sadness, anxiety, and fatigue that can hinder their ability to successfully engage in everyday responsibilities, such as self-care or caregiving for others.1
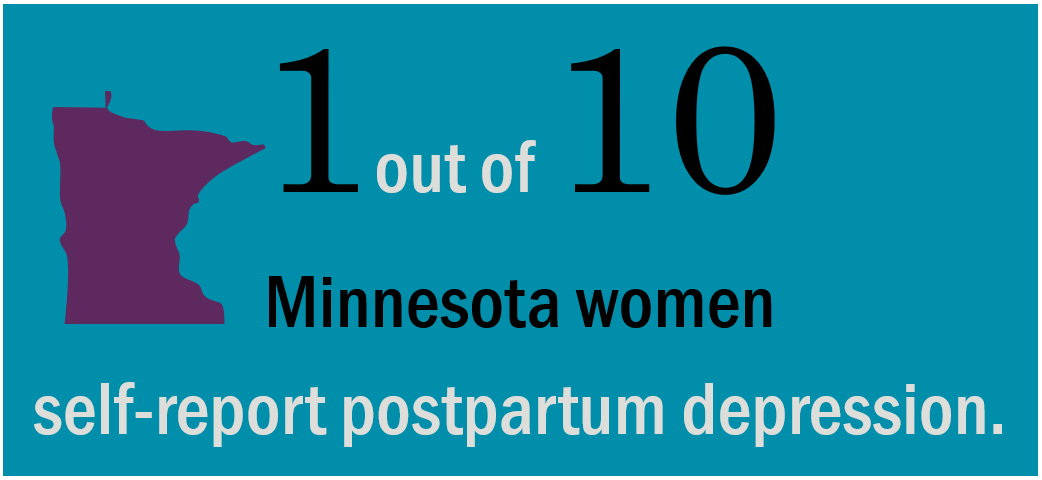
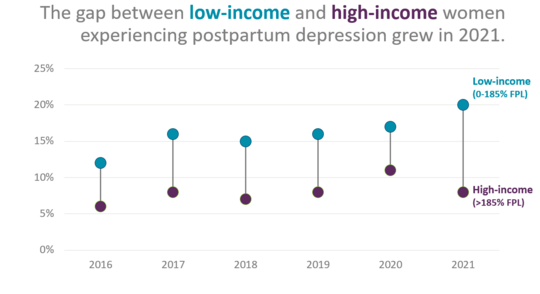
Although the 2021 prevalence of PPD in Minnesota (11%) was lower than the U.S. rate overall (13%), MN PRAMS data showed significant disparities in self-reported PPD. In Minnesota, self-reported PPD differs by several factors, including race, income level, and type of insurance. For example, combined data collected from 2016-2021 showed that the percentage of U.S born African American women who self-reported PPD were two times higher than white women (18% versus 9%, respectively) and for American Indian women, the percentage of self-reported PPD was almost three times higher than the percentage for white women (22% versus 9%). Additionally, the percentage of low-income respondents (those at or below 185% Federal Poverty Level (FPL)) who self-reported PPD was two times higher compared to high-income respondents (those above 185% FPL). In 2021, there was a significant increase in income disparity within PPD, resulting in the widest gap observed over a six-year period (Figure 1).
Figure 1- Income disparity among pregnant people with postpartum depression over time, 2016-2021
 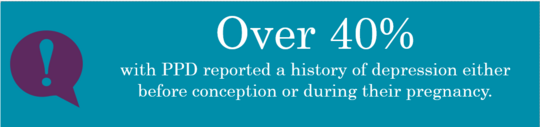
The MN PRAMS data also indicated a greater proportion of pregnant people who self-reported PPD also indicated a prior history of self-reported depression either three months before conception or during pregnancy. These findings demonstrate that preconception care offers potential opportunities to identify and treat depression earlier, with the aim to minimize adverse outcomes during and after pregnancy. Here, a MN PRAMS respondent's testimony highlights the benefits of addressing depression earlier to help prevent PPD during subsequent pregnancies.
 |
|
“This was my second pregnancy, and I had a much different experience than with my first in many ways. First, I had a wonderful "care team" around me; psychiatrist, therapist, OB-GYN, and family doctor who ensured I was prepared to give myself the best chance at not having severe depression during and after pregnancy. I had difficult PPD with my first and took many years to be okay. With my care team and medications, I was able to have a much better pregnancy (emotionally) and have NOT had PPD.” – MN PRAMS respondent |
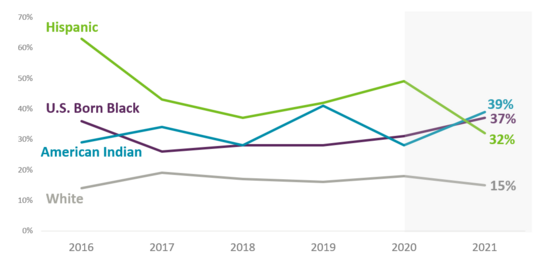
Although a preconception visit can offer an opportunity for early identification and treatment of pregnant people with depression, many individuals still encounter barriers to accessing care before, during, and after pregnancy. Our analysis of the 2016-2021 combined data indicated nearly one in four women said that they did not have a healthcare visit in the 12 months leading up to their pregnancy. Disparities were observed with income. The percentage was more than three times higher for low-income respondents (those at or below 185% FPL) who reported not have a healthcare visit 12 months before conception compared to higher income respondents (those above 185% FPL) (38% versus 12% respectively). Combined 2016-2021 data showed 45% of Hispanic women reported not having a healthcare visit 12 months before pregnancy and 41% of them said this was because they didn't have health insurance to cover the cost of the visit. Furthermore, the disparity of those not seeking healthcare check-ups within 12 months prior to pregnancy widened between 2020 and 2021 among women belonging to the U.S. born Black and American Indian populations (Figure 2).
Figure 2- Women who did not have a health care visit 12 months before pregnancy by race over time
Structural or financial challenges were prevalent within the healthcare system. Of women who did not get prenatal care as early as they wanted, 29% reported that they could not get an appointment when they wanted one, 27% said the doctor or their health plan would not start care as early as they wanted, 18% said they did not have enough money or insurance to pay for their visits, 15% said they didn't have their Medicaid, Medical Assistance, or MNCare card, and 10% said they did not have any transportation to get to the clinic or doctor's office. Some of the similar obstacles, in terms of structure and finances, were encountered in the context of preconception care. By mitigating these barriers, it is possible to enhance access to care for women and proactively address depression during its initial stages, prior to childbirth. Following is a quote from a MN PRAMS respondent sharing their perspective about women with less resources, given their experience with depression.
 |
|
“I had debilitating depression plus anxiety during my first trimester. I have resources to manage this (good health insurance, supportive family, etc.) but it was HARD. I think attentiveness to mental health during and after pregnancy could be enhanced. I could see this problem in women with less resources being very dangerous for mom and baby.” – MN PRAMS respondent |
Furthermore, there is potential to enhance healthcare professionals and patient discussions around improving health and addressing depression before pregnancy. Though the American College of Obstetricians and Gynecologists recommends screening everyone receiving well-woman, pre-pregnancy, prenatal, and postpartum care for depression2, approximately 30% of MN PRAMS respondents still reported not being asked if they were feeling down or depressed during a health care visit in the 12 months before they got pregnant. Here are some remarks provided from MN PRAMS respondents.
 |
|
“Being a pediatrician myself, I feel there is a lot of missed opportunities for lactation learning and postpartum depression. I spend a lot of time talking about these subjects with the mother when I am not their PCP.” – MN PRAMS respondent
“Throughout pregnancy I was offered questionnaires to assess for postpartum depression, but I was rarely given time to fill it out and no one ever reviewed them or discussed them with me.” – MN PRAMS respondent
|
Stressors and postpartum depression
Women were asked on the MN PRAMS survey if they experienced these specific types of stressors during the 12 months before their baby was born:
-
Emotional: Includes ill family member, a loved one died.
-
Financial: Includes moved to new address, lost her job, could not pay bills, husband/partner lost job, and husband/partner/self had a cut in work hours or pay.
-
Partner: Includes divorce, argued with husband/partner, husband/partner did not want the pregnancy, and abuse from husband/partner.
-
Trauma: Includes homelessness, someone close used alcohol/drugs, husband/partner/self in jail.
Analysis of 2016-2021 data indicates a higher percentage of women with PPD also experienced more emotional, financial, partner, and trauma stress compared to women without PPD (Figure 3). They also experienced a higher number of stressors compared to women without PPD. The percentage of women with PPD experiencing five or more stressors was three times higher than women without PPD.
Figure 3- Postpartum depression and stressors 2016-2021
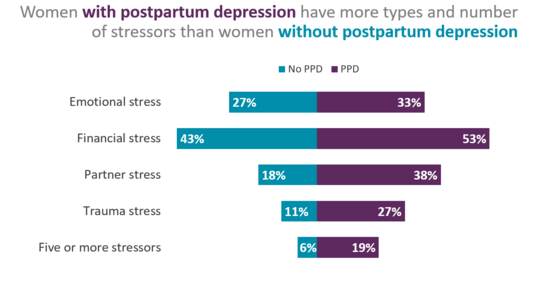 U.S. Born Black and American Indian women face more stressors than women of other races. According to Figure 4, 21% of U. S. born Black women and 29% of American Indian women experienced five or more stressors, in contrast to only 7% of white women, 5% of Hispanic women, and 3% of women from other racial backgrounds.
Figure 4- Five or more stressors by race 2016-2021
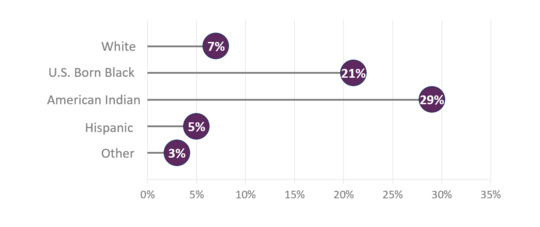 Individuals with elevated stress levels may experience exacerbated effects from racial discrimination. About one out of four U.S. born Black women and American Indian women reported they felt emotionally upset (for example, angry, sad, or frustrated) because of how they were treated based on their race in the 12 months leading up to the birth of their newborn. Further, approximately 7% of U.S. born Black women and 8% of American Indian women reported they experienced discrimination by healthcare providers during their prenatal care, labor, or delivery based on their race, ethnicity, or culture.
Women who experienced PPD also reported higher percentages of stress due to racial bias in the 12 months prior to birth or discrimination by healthcare providers during prenatal care, labor, or delivery compared to women who did not experience PPD (17% vs 5% and 4% vs 1% respectively).
 |
|
“They were always asking me about smoking or drinking, I think they did it because I'm African American. They asked at every appointment, and it felt like they were just so sure that I was doing something. It was very stressful. They're going to test the baby when it's born anyway so it would be better if they could just ask once. I went to school for public health and sociology, so I see things through a different lens, and I really felt like it was because of my race. It was stressful.” – MN PRAMS respondent |
The pressure of racism and discrimination can have a detrimental impact on various aspects of a woman's care experience, ultimately resulting in decreased trust and avoidance of seeking necessary care. In general, eliminating discriminatory policies, educational practices, structural and financial barriers to care, especially before pregnancy, can create more opportunity for all women to receive equitable access to quality healthcare and help reduce stress for women with PPD.
Treatment
Depression is treated with therapy, medicine, or a combination of the two3. It is important to acknowledge the MN PRAMS phase 8 survey solely focuses on counseling, specifically for depression or anxiety, rather than depression alone. Combined 2016-2021 data indicated 24% of women who self-reported PPD in the postpartum period received counseling for depression or anxiety compared to 7% who did not self-report PPD.
Our new phase 9 survey includes improved questions to enable us to assess diagnosed PPD as well as treatment specifically for PPD (medication, counseling, or both). Our Social Determinants of Health (SDoH) supplement from the previous year, will also provide valuable insight on the need for mental health services and obstacles to accessing mental health services.
 |
|
“I think there needs to be more services to those struggling with depression/anxiety, more counseling that is easy to schedule, and at places that are easy to get to. And, maybe kid friendly if they have more kids.” – MN PRAMS respondent |
The following recommendations were made based on analysis results of MN PRAMS data on PPD:
- Providers and healthcare systems should address structural and systemic barriers to accessing healthcare and mental health services before, during, and after pregnancy.
- Providers should talk about depression with patients, particularly before pregnancy.
- Healthcare systems should Identify and address racism in healthcare.
- Medical education should focus on inclusion and addressing bias in their curriculum.
- Healthcare providers, mental health professionals, and clinic social workers should provide women with resources and support to help address or eliminate stressors throughout the life course and particularly before pregnancy.
-
Women should ask friends and family for support during stressful times.
- Women should talk to their healthcare provider as soon as possible if they suspect they have depression.
1. March of Dimes: Postpartum Depression
2. The American College of Obstetricians and Gynecologists (ACOG): Patient Screening
3. Office on Women: Depression
|