Attention Behavioral Health Providers: KEPRO Atrezzo Submission Requirements Update
Maine Department of Health & Human Services sent this bulletin at 05/31/2018 03:03 PM EDT Having trouble viewing this email? View it as a Web page.
Having trouble viewing this email? View it as a Web page.
Attention Behavioral Health Providers: KEPRO Atrezzo Submission Requirements Update
Effective June 1, 2018, KEPRO, in collaboration with the Office of MaineCare Services, has updated the submission requirements within the Atrezzo system. These changes are being made to ensure that authorizations for services do not include any dates in which the member was ineligible for the service in question.
Please see the updated submission requirements:
- All requests for authorization must be submitted no sooner than ten calendar days prior to the service start date. Additionally, authorizations can only be backdated up to five calendar days prior to the submission date of a prior authorization request. There will be no exceptions to this submission requirement.
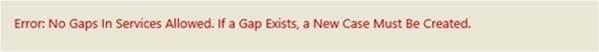
- Any submission with a gap of more than five calendar days from the preceding authorization end-date will result in an error message and require that the provider submit a new request in Atrezzo. This will generate a new authorization number.
Atrezzo Error Message:
If a member does not have MaineCare at the time of service, a courtesy review is required as a placeholder in Atrezzo and allows for a determination of medical necessity. If the member is deemed medically eligible, in the event the member becomes MaineCare eligible, then the approved services can be covered by MaineCare. If a courtesy review is not entered into the portal at the time of service, then the review request can only be backdated up to a maximum of five calendar days from the date of submission. Please note that courtesy reviews are not available for Opioid Health Home services.
If you have any questions, please contact KEPRO Provider Relations at (866) 521-0027 or email.
