|

Alaska Department of Health and Social Services Weekly COVID-19 and Influenza Update
May 22–May 28, 2022
Key Findings
- COVID-19 transmission remained widespread in most parts of Alaska during the week of May 22–May 28, 2022, with evidence for increasing cases in some areas but decreases elsewhere.
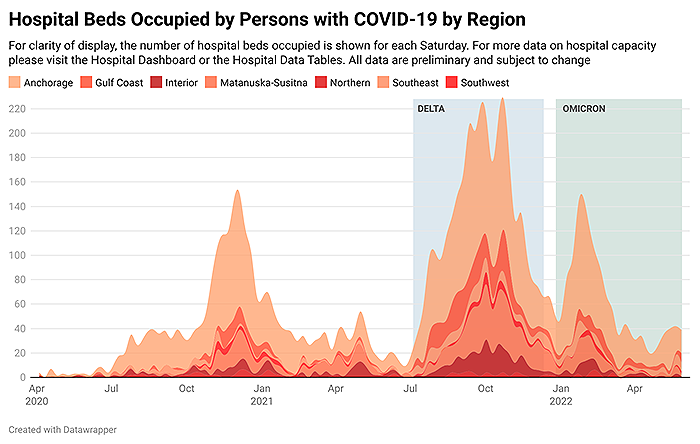
- The number of patients hospitalized with COVID-19 has increased modestly over the past few weeks (see graph below illustrating hospital beds occupied by persons with COVID-19).
- Detected influenza cases slightly decreased the week of May 22–May 28 compared to the previous week.
- Other respiratory viruses are circulating in addition to SARS-CoV-2 and influenza virus.
COVID-19
COVID-19 Case Trends
- COVID-19 transmission continues to occur widely throughout much of Alaska, with a modest upwards trajectory. Cases and hospitalizations remain substantially below the peak of the Omicron wave, though COVID-19 hospitalizations have increased over the past few weeks.
- 2,054 cases were reported in Alaskans the week of May 22–May 28, which is a 24% increase compared to the previous week. (This increase reflects both a modest true increase as well as cases that occurred in previous weeks but were reported belatedly to the Section of Epidemiology.)
- COVID-19 cases continue to rise in the four largest boroughs (Municipality of Anchorage, Matanuska-Susitna Borough, Fairbanks North Star Borough, and Kenai Peninsula Borough). The increases in reported cases last week from Fairbanks North Star Borough and Matanuska-Susitna Borough reflect both true increases as well as delayed reports from prior weeks. The number of reported COVID-19 cases last week among City and Borough of Juneau residents declined for the first time after 6 weeks of increases, but it is too soon to determine whether Juneau is on a sustained downward trajectory.
- The intensity of COVID-19 transmission varies between communities outside the largest boroughs. Trajectories are mixed, with COVID-19 cases declining in some communities but increasing in others. There is no clear overall trajectory in Southeast Alaska, though per capita incidence remains high in many parts of the region and some of the less populous parts of Southeast Alaska in particular have experienced recent increases in cases. Making comparisons between communities is difficult because testing practices may vary between communities.
- COVID-19 cases continue to occur in many communities in western Alaska off the road system and some communities have high incidence relative to their population size.
- The Omicron variant accounts for effectively all SARS-CoV-2 circulating in Alaska. The BA.2 lineage (a sub-type of Omicron) accounts for nearly all sequenced specimens. The BA.2.12.1 sub-lineage has been found in Alaska and is increasing in frequency. Visit Alaska’s SARS-CoV-2 Genomics Dashboard to learn more.
- To learn more about COVID-19 cases, hospitalizations, and deaths due to COVID-19 in Alaska, visit the Cases Dashboard or the quarterly report. The cases dashboard includes demographic information on cases and the quarterly report includes demographic information on hospitalizations and deaths.
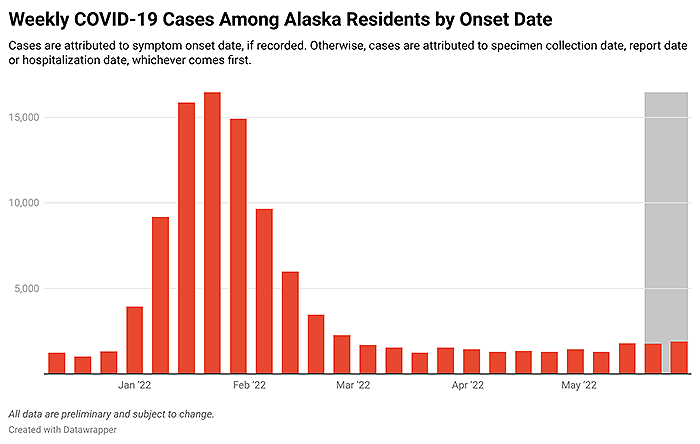
COVID-19 cases among Alaska residents by week of onset date.
Click here to sort data.
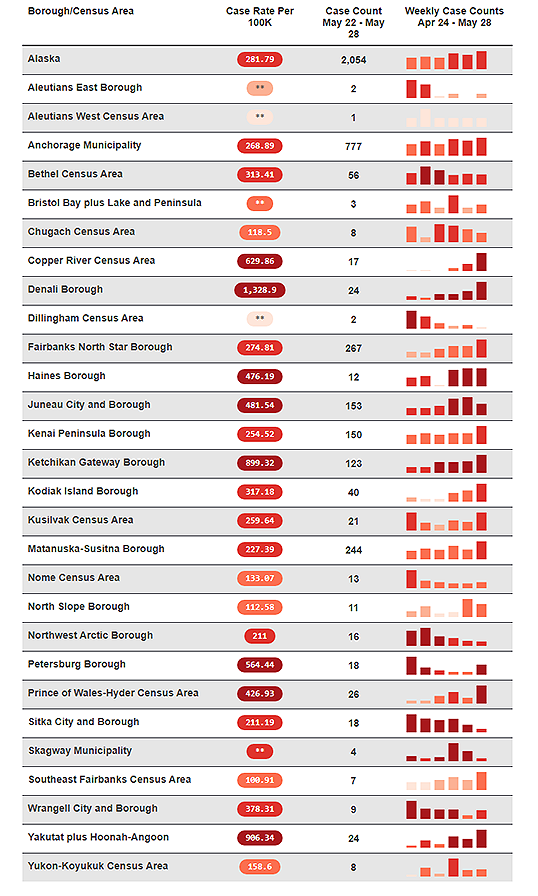
*Rates based on <20 observations are statistically unreliable and should be used with caution.
**Rates based on <6 observations are not reported.
Community case rates are based on case report date.
COVID-19 and Hospital Capacity
- Some regions continue to experience capacity limitations because of large numbers of patients overall (not necessarily with COVID-19 or other respiratory viruses) or due to staffing issues. However, recent inpatient volumes in more urban areas have created some minor limitations in referral capacity for higher-level and specialty care.
- Patient Care Strategies for Scare Resources are being discussed actively at multiple institutions given a growing concern for the shortage of infant formula and iodinated contrast dye, which is needed for CT scans, heart cauterizations, and other vascular procedures. The Crisis Care Committee will be engaged in facilitating these discussions as this situation evolves.
- As of June 1, 2022, there were 49 persons with COVID-19 in Alaska hospitals, accounting for 4.1% of all hospitalized persons. Visit the Hospital Dashboard for more data.
COVID-19 and Vaccination
- 72.3% of Alaska residents aged ≥5 years have received at least one dose of a COVID-19 vaccine. Among those who completed the primary vaccine series, 51.7% of Alaska residents ≥18 years have received their booster. Learn more about COVID-19 vaccination coverage in Alaska on the Vaccine Dashboard. Learn more about COVID-19 vaccines.
- Vaccines help protect against infection and against severe disease, especially when a person is up to date on vaccinations. During recent weeks, the number of documented hospitalizations due to COVID-19 was too small to estimate statistically reliable incidence rates by vaccination status. However, evidence from previous time periods when the Omicron variant was dominant shows that the incidence of hospitalization was lowest in persons up to date on COVID-19 vaccination.
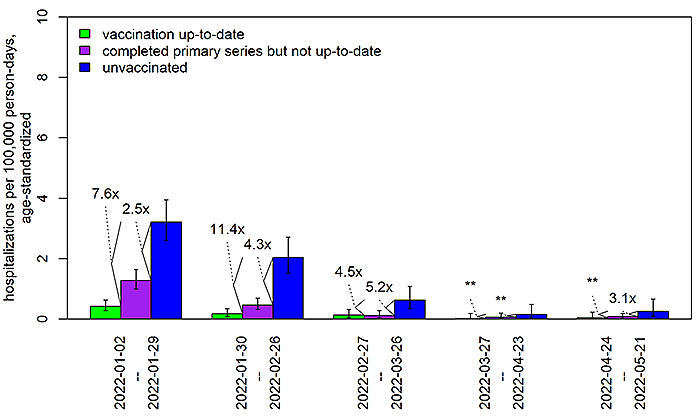
In order to more easily identify changes over time, the definition of “up to date” as of May 24, 2022, was applied to data from all time points. **Especially when rates are very low, the estimates of fold-differences between rates may be imprecise. Fold-differences are not calculated if one of the rates is based on <6 cases.
- Among Alaska residents aged ≥5 years from January 16, 2021–May 28, 2022, 79,425 cases were documented in persons who had completed the primary series and were considered fully vaccinated. Among those vaccine-breakthrough cases, 559 hospitalizations and 204 deaths due to COVID-19 have been recorded. During that time, 103,136 cases have been documented in unvaccinated Alaskans aged ≥5 years, leading to 1,880 hospitalizations and 681 deaths. All data are preliminary and subject to change.
- During the Omicron wave, the incidence of COVID-19 cases in vaccinated persons has become more similar to the incidence in unvaccinated persons. This trend likely reflects multiple factors which may include: immunity wanes over time, cases in vaccinated persons may be more likely to be detected than cases in unvaccinated persons, and there may be increased infection-induced immunity especially among unvaccinated persons.
- One way to monitor how well vaccines are working is to perform a test-negative case-control analysis, which compares the vaccination status among people who test positive to the vaccination status among people who test negative. In an analysis of testing of symptomatic children and adults at schools in Alaska during January through March 2022, persons who were up to date on COVID-19 vaccination were 61% less likely to test positive than those who were unvaccinated. See the quarterly report to learn more.
Influenza (“Flu”)
- Reported influenza cases began increasing in Alaska in mid-December but declined during January and remained relatively flat through February and March. Cases began increasing in April, with the number of reported cases the week of May 22–May 28 decreasing from the number reported the previous week.
- Right now, most influenza in Alaska is caused by influenza A.
- 24% of Alaskans aged ≥10 years have been vaccinated against seasonal influenza. It is not too late to get vaccinated against influenza.
- Learn more in the weekly Alaska Influenza Snapshot.
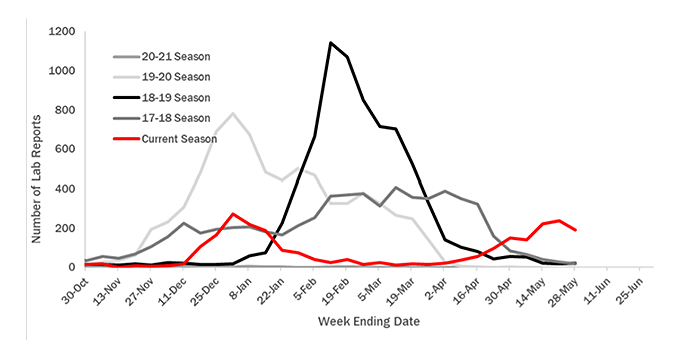
Positive influenza lab reports in Alaska by week of specimen collection for the 2017-2018 influenza season through present. The current season through May 28, 2022 is shown in red.
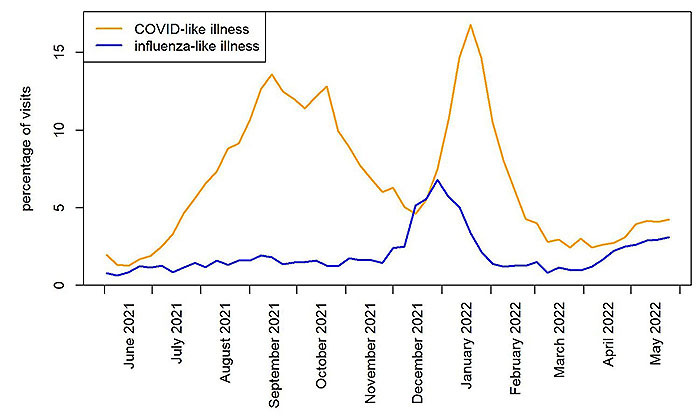
Emergency Department Visits with COVID-like or Influenza-like Illness
- Syndromic surveillance consists of analyzing data on symptoms and diagnoses among patients visiting emergency departments in Alaska. The main goal is to identify trends. Unlike case-based surveillance, syndromic surveillance does not depend on laboratory testing.
- Influenza-like illness (ILI) is defined as having a fever and at least one other symptom, such as a cough or sore throat. Patients with a diagnosis of influenza are also included, regardless of symptoms. (The graph of ILI in the weekly influenza snapshot differs because the definition of ILI used therein is based solely on symptoms and does not include diagnostic codes.)
- COVID-like illness (CLI) encompasses a broader array of respiratory and other symptoms than influenza-like illness. This category also includes any patient with a diagnosis of COVID-19, regardless of symptoms.
- Patients with a diagnosis of COVID-19 are excluded from the ILI category and, likewise, patients with a diagnosis of influenza are excluded from the CLI category. (In the rare instances in which a patient is diagnosed with both influenza and COVID-19, they are included in the CLI category). A patient without a diagnosis for either could be included in both the CLI and ILI categories, depending on the patient’s symptoms. CLI and ILI may be caused by respiratory viruses other than SARS-CoV-2 and influenza virus.
- As the Delta variant wave waned in Alaska in late October and November 2021, the percentage of emergency department patients with CLI declined. However, it increased in mid-December, reaching its peak in mid-January. Now, it is at a level lower than that observed in December before the Omicron wave. The percentage of emergency department patients with CLI the week of May 22–May 28 was similar to the percentage recorded the prior week.
- ILI levels increased in December and peaked in late December 2021 and early January 2022. During April 2022, ILI levels increased again. The ILI level last week remained similar to the percentage reported the previous week.
New updates to protect yourself and your family
-
Treatments for COVID-19 are available and work best when given as soon as possible after symptoms start. If you test positive and you’re at increased risk for severe COVID-19, ask a health care provider about treatment options. If you have COVID-like symptoms but test negative on an at-home test, you could still have COVID-19. To be sure, either test again with an antigen test 2 days after your first test or consider getting a molecular test as soon as possible if you are at high-risk for complications. Learn more about COVID-19 treatments and where you can find COVID-19 treatments.
-
Vaccine boosters: Everyone 5 or older should get a COVID-19 vaccine booster if it's been five months since receiving the Pfizer or Moderna vaccines or two months since receiving the Johnson & Johnson vaccine. People over the age of 50 and some immunocompromised individuals should receive a second mRNA booster (Pfizer or Moderna) four months after their first booster dose. To be considered up to date on COVID-19 vaccination, get recommended boosters when eligible. Additionally, people who have received the Johnson & Johnson vaccine for both their primary dose and booster dose may receive a second booster dose using an mRNA vaccine. Pfizer or Moderna vaccine boosters are preferred. Individuals aged 5-17 can receive a Pfizer booster only.
Information and Resources
- The State of Alaska COVID-19 vaccines update page
- The State of Alaska COVID-19 information page provides more information about the virus and how individuals and businesses can protect themselves and others from transmission.
- The DHSS Business and Employer Toolkits page has communications resources for any organization that wants to keep workers, partners, clients, and customers informed about COVID-19.
- DHSS COVID-19 Communication Toolkit provides PSAs, flyers, and social media graphics.
- Subscribe to the DHSS Insights blog for behind-the-scenes news about Alaska’s COVID-19 response and other efforts to protect the health and well-being of Alaskans.
- DHSS offers free presentations upon request to groups about COVID-19, the vaccines, COVID-19 prevention, or other health topics upon request. Learn more or request a presentation on our Speaker’s Bureau web page.
- For the most up-to-date case information, see the Alaska COVID-19 Information Hub dashboard: data.coronavirus.alaska.gov. All dashboard data are updated Wednesdays (except holidays).
- For DHSS media inquiries, please contact clinton.bennett@alaska.gov
ECHO sessions

Session information and recordings of previous ECHO sessions
subscribe to ECHO calendar updates | email: echo@alaskachd.org | website: akecho.org
ECHO sessions create virtual learning communities by connecting Alaska's health experts with specific audiences on specific topics. These sessions are produced and facilitated by UAA’s Center for Human Development Alaska ECHO project in partnership with the State of Alaska, Department of Health & Social Services.
The full schedule of ECHO sessions and access to COVID-19 ECHO videos and slideshows are available for download anytime on the DHSS ECHO web page. Several ECHO sessions have ended for the summer. Please continue to check the schedule for when they will return in the fall.
|